26-year-old female with a diagnosis of major depressive
Patient 1:
26-year-old female with a diagnosis of major depressive disorder and social anxiety disorder who is increasing in isolation and poor self-care. She is in her third trimester of pregnancy.
Patient 2:
16-year-old male with a diagnosis of major depressive disorder, severe. He has seen a therapist weekly for the past 6 months and has had minimal change in symptoms. He has expressed thoughts of wanting to die.
Patient 3
: 72-year-old male with diagnosis of major depressive disorder and panic disorder. He has cardiac history and takes antihypertensive medications.
Patient 4
: 8-year-old Asian female with a diagnosis of severe depressive disorder presents to the office with a report of worsening symptoms. She has never taken psychotropic medication before.
Step 2:
Create
a Medication Guide for a patient. In your guide, you should provide the following specific instructions for the patient:
Describe the chosen classification of medications, from the classification category, for your chosen vulnerable patient. Explain your rationale for your choice.
Explain what dose you would start the chosen medication with and the frequency.
Discuss how the medication works to treat their symptoms.
Explain how long they should take the medication.
Discuss the typical or common side effects of the medication.
Explain the urgent or emergent considerations for the patient taking the medication.
The Medication Guide should also include:
Directions you would provide the patient on how to take the prescribed medication
Instructions on what the patient should do if a medication dose is missed
List of any other medications, over-the-counter medications, and/or supplements/herbals the patient should avoid while taking the prescribed medication
List of foods the patient should avoid when taking this medication
Date when the patient should return for follow-up visit with you
Discussion about the legal and ethical considerations for the medication being prescribed
Answers in consideration of Social Determinants of Health on how you would:
Assist the patient who cannot not afford to pay financially for the medication you are recommending/prescribing; and/or
Has difficulty with transportation that impacts their ability to present for regular appointments with you
Discuss how financial hardship and lack of transportation could relate to Social Determinants of Health, as well as why they are important considerations for you as a prescriber.
Sertraline Medication Guide for Pregnant Patients With Depression
This medication guide is designed for a pregnant patient in her third trimester diagnosed with major depressive disorder and social anxiety disorder. Sertraline, an SSRI, is widely recommended as a first-line treatment in pregnancy due to its strong safety profile and effective symptom reduction. This guide explains how the medication works, how to take it, possible side effects, and important legal and ethical considerations relevant to prescribing psychotropics during pregnancy.
Sertraline belongs to the Selective Serotonin Reuptake Inhibitor (SSRI) class. SSRIs increase serotonin availability in the brain, helping regulate mood, motivation, and anxiety. SSRIs are considered first-line therapy for perinatal depression due to their extensive research support and lower risks compared to tricyclic antidepressants or benzodiazepines (ACOG, 2021; Stewart, 2020).
Why Sertraline?
-
Best-studied SSRI in pregnancy
-
Low placental transfer compared to other SSRIs
-
Low neonatal adaptation risk
-
Effective for both depression and social anxiety
-
Fewer cardiac concerns than paroxetine or citalopram
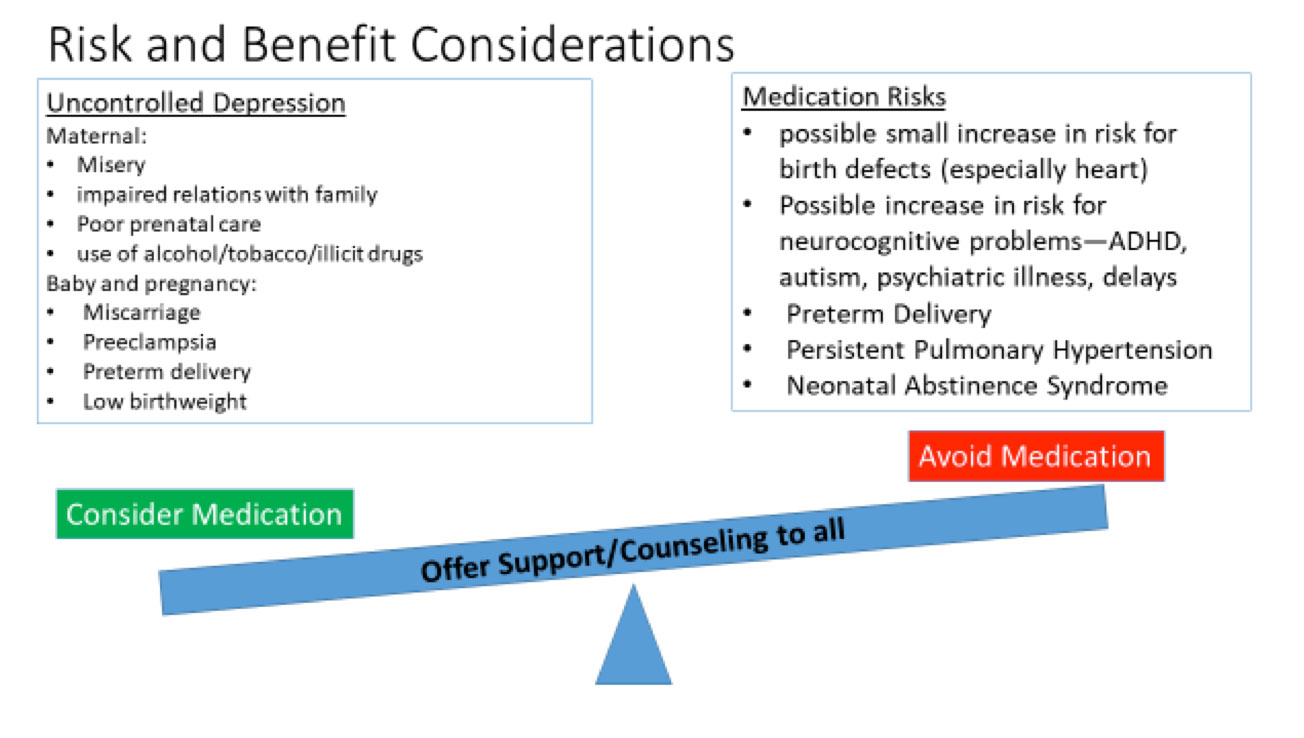
Given the severity of symptoms and risk of functional decline, initiating an SSRI is clinically appropriate and safer than untreated maternal depression, which increases risks of preterm labor, low birth weight, and impaired bonding postpartum.
For pregnancy, a low starting dose is recommended.
Starting dose:
-
Sertraline 25 mg orally once daily for 7 days
-
Increase to 50 mg once daily thereafter
Doses may be gradually increased (up to 150–200 mg/day) depending on symptom response.
Sertraline blocks the reuptake of serotonin at the neuronal synapse, increasing serotonin availability in the brain. Benefits include:
-
Improved mood stability
-
Reduced anxiety symptoms
-
Decreased intrusive negative thoughts
-
Enhanced energy and motivation
-
Improved functioning in social contexts
Patients typically begin to see improvement within 2–4 weeks, with full therapeutic effects by 6–8 weeks (Gorman et al., 2022).
The patient should take Sertraline for at least 6–12 months after symptom improvement. Since she is pregnant, consistent treatment throughout the postpartum period is particularly important due to the high risk of postpartum depression.
The medication should never be stopped abruptly. Dose tapering is required under medical supervision.
Most side effects are mild and improve within 1–2 weeks.
Common effects include:
-
Nausea
-
Mild insomnia
-
Headache
-
Dry mouth
-
Decreased appetite
-
Increased sweating
Seek immediate medical attention for:
-
Suicidal thoughts or worsening depression
-
Severe agitation or restlessness
-
Allergic reaction (rash, swelling, difficulty breathing)
-
Serotonin syndrome (confusion, fever, tremors, diarrhea)
-
Changes in fetal movement
-
Unusual bleeding or bruising
Neonatal adaptation syndrome is rare but possible; symptoms may include mild irritability or jitteriness after delivery.
How to Take the Medication
-
Take once daily, preferably at the same time each morning.
-
Can be taken with or without food.
-
Do not crush or chew tablets.
If a Dose Is Missed
-
Take the missed dose within 4–6 hours.
-
If close to the next dose, skip the missed dose—never double-dose.
Medication and Supplement Interactions
Avoid:
-
MAOIs
-
Triptans
-
St. John’s Wort
-
Tramadol
-
Linezolid
-
NSAIDs (increased bleeding risk; use with caution)
Foods to Avoid
No major dietary restrictions, but avoid excessive alcohol and herbal teas marketed for “mood enhancement.”
The patient should return in:
-
2 weeks after initiation to evaluate side effects and safety
-
4–6 weeks for dose adjustment
-
Monthly thereafter until stable
Postpartum follow-up is essential for relapse prevention.
Prescribing SSRIs during pregnancy involves balancing maternal and fetal risks. Ethical principles include:
Beneficence
Treating maternal depression reduces risks of poor prenatal care, suicide, and impaired infant attachment.
Nonmaleficence
Sertraline presents minimal fetal risk; untreated depression is riskier.
Autonomy
The patient must be fully informed about risks, benefits, alternatives, and the option to decline medication.
Justice
The provider must ensure equitable access to treatment regardless of socioeconomic status.
Documentation should reflect informed consent, shared decision-making, and discussion of pregnancy-specific risks.
Financial Hardship
If the patient cannot afford Sertraline:
-
Provide generic formulation to reduce cost
-
Connect patient with Medicaid or pharmaceutical assistance programs
-
Utilize community mental health pharmacy programs
-
Offer samples when available
Affordable medications reduce non-adherence and prevent relapse.
Transportation Barriers
If the patient has difficulty attending appointments:
-
Offer telehealth follow-ups
-
Coordinate virtual check-ins with OB providers
-
Connect with transportation assistance (Medicaid rides, local nonprofit support)
-
Extend prescription duration to 60–90 days when safe
Why Social Determinants Matter in Prescribing
Financial stress and transportation problems increase the risk of medication non-adherence, missed appointments, worsened depression, and poorer maternal-fetal outcomes (WHO, 2022). As a prescriber, addressing SDOH ensures equitable, safe, and effective care.
Sertraline is an evidence-based, safe, and effective treatment for pregnant patients with major depressive disorder and social anxiety disorder. With proper dosing, monitoring, education, and consideration of individual social needs, it can significantly improve maternal well-being and reduce perinatal risks. A holistic, ethical, and patient-centered medication plan will support both maternal and fetal health during pregnancy and postpartum.
American College of Obstetricians and Gynecologists. (2021). Treatment of perinatal mental health conditions.
Bianco, M., & Yonkers, K. (2020). Management of depression during pregnancy. New England Journal of Medicine, 383(6), 552–560.
Gorman, J. M., et al. (2022). SSRIs for depression and anxiety: Mechanisms and outcomes. Journal of Clinical Psychiatry, 83(4), 1–8.
Huybrechts, K. F., et al. (2020). SSRI safety in pregnancy. BMJ, 368, 1–12.
Koren, G., & Ornoy, A. (2021). Antidepressants in pregnancy: Updated safety data. Reproductive Toxicology, 103, 134–142.
Molenaar, N. M., et al. (2020). Perinatal depression treatment outcomes. The Lancet Psychiatry, 7(6), 498–509.
National Institute of Mental Health. (2021). SSRIs and pregnancy.
Stewart, D. E. (2020). Clinical practice guidelines for perinatal depression. CMAJ, 192(11), E310–E316.
World Health Organization. (2022). Social determinants of mental health.
Yonkers, K., et al. (2021). Managing psychiatric medications during pregnancy. Obstetrics & Gynecology, 138(5), 871–883.